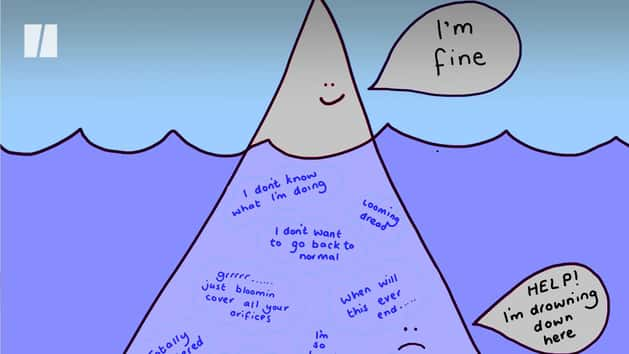
Many impacts of the coronavirus pandemic are easy to see, from facemasks and visors to closed restaurants and shops to deserted high streets. But there’s one consequence of this wretched virus, the one I fear most, that cannot be seen – its devastating impact on our mental health.
It’s become increasingly clear that lockdown is the perfect storm for our mental health. Is it any wonder, when we’ve faced nearly a year of living a dramatically different lifestyle, with no foresight as to when it will all end?
People from all walks of life have relayed their mental health struggles throughout the pandemic, so on behalf of the medical community, I feel inclined to speak out. As a doctor, I am acutely aware of benefits this can bring – but I won’t pretend my struggles are easy to admit.
When training as a doctor, I knew my job would be hard – long hours, difficult decisions, breaking bad news – but I never imagined it would affect my mental health as it did. I took my first period of sick leave during my Foundation Year 1, and my problems followed on from there. I kept thinking that once qualified, I would finally be able to work on my mental health, by following a routine and ensuring I took time to switch off.
“Mental health struggles are not uncommon amongst the medical community, with one survey found 85% of doctors have experienced issues with their mental health.”
But being a GP presented itself with new mental challenges. Often, patients offload their anxieties onto their GP, so you sometimes feel as though you’re doing the job of therapist as well as doctor. This a natural part of the role and one which I graciously accept, but sometimes, it’s an emotionally taxing demand. It’s hard to keep filling up everyone else’s cup, whilst yours is completely empty.
Mental health struggles are not uncommon amongst the medical community, with one survey found 85% of doctors have experienced issues with their mental health. As we near the end of the most exhausting year the NHS has seen, I would anticipate this figure to now be even higher.
You might not expect the pressures to filter down to primary care. You will have seen in the media how, when the first wave came, those infected with Covid-19 needed hospital admissions and ventilators, which was a true and saddening reality. Yet those cases were not in the majority – many thousands of people infected with the virus were well enough to stay at home and be managed by their GP. How long will it last? How do I self-isolate? When can I see my loved ones again? For many weeks, we in the healthcare community spent our time attempting to ease these concerns, while knowing next to nothing ourselves.
It was incredibly hard, especially for anyone already struggling with their mental health. Having lived with depression for so long, I know when I’m headed towards a low and have learned exactly how to manage it – I spend time with my friends, I go to a café to read, or go see a film. But in lockdown, I couldn’t do any of these things. I feared I would become so sick that I would have to stay home, unable to treat my patients – and unable to treat myself.
“For the sake of the 1.4million NHS workers, our industry needs to change.”
Thankfully, I work at a surgery where I’ve been able to be honest about my struggles from the offset. Our practice is technically advanced, with a superb digital triage system, Doctorlink, that helps us prioritise the patients in most need of care and so reduce administrative burden.
But this isn’t common amongst my peers. For many, the sudden shift to technology at the outbreak of the pandemic was wholly new and an additional struggle, but the response from senior management at some surgeries was simply to ‘be more resilient’. I was lucky to be supported, but I still struggled – I can only imagine how my colleagues in less prepared environments have coped.
I know I am good at my job and I love nothing more than helping my patients, but for the sake of the 1.4million NHS workers, our industry needs to change. Firstly, there needs to be a systemic implementation of the digital support systems I have seen first-hand alleviate the burden not just on the system, but on the doctors who provide crucial care. Secondly, there needs to be an attitudinal shift. I have always been able to open up to my managers about my problems, but not everyone is so lucky – stigmas still remain.
To get through this crisis, and those which will surely come, GPs must feel more comfortable to be honest about their mental health struggles. We must not be overlooked in the mental health epidemic. If we are, the very system responsible for getting the nation through this crisis will be at risk of its own collapse.
Dr Steph Colbourn is a GP at Portland Medical in Croydon, London
Have a compelling personal story you want to tell? Find out what we’re looking for here, and pitch us on ukpersonal@huffpost.com